- Diabetic foot Exams
- Diabetic Footwear
- Wound care
- Custom orthotics
- Digital radiographs
- KeryFlex Nail Replacement
- Q-Clear Laser
- Surgical consultations

KeryFlex is a painless, in-office application at Podiatry of Chicago that restores the appearance of an individual’s natural nails. This system allows for the foot doctors at Podiatry of Chicago to remodel an individual’s damaged nails affected by fungus, defects or trauma. The composite resin creates a flexible, but durable, non-porous nail that allows the remaining natural nail to grow. The KeryFlex nail is an immediate cosmetic improvement providing a natural-looking nail. KeryFlex in office nail restoration will give you confidence in toe-nails you will be proud of.

Leneva Injections
Leneva is an innovative human allograft adipose tissue that is injected into an area that is lacking cushioning or fat. It helps your body to turn the injected substance into your own fat with the goal of helping offload the area.
What is Leneva Used for:
- There are multiple indications for adipose injections but what we mainly use them for in podiatry is to add fat or cushioning to an area on the foot that is irritated from a lack of fat, fat pad atrophy or a displaced fat pad.
- As we age the fat stores in our skin deplete leaving us with less cushioning, which on the bottom of the foot is needed to help us walk without pain. If an area gets too much pressure from a lack of fat then pain, a callus or pressure ulceration can develop.
What to Expect:
- Once our doctors decide that a Leneva injection could be a beneficial procedure for you, they will numb the affected area with a small amount of anesthetic. Once numb the allograft adipose is injected to the area.
- The patient will be required to stay off the foot in our office for 30 minutes post- injection to ensure the substance does not disperse to a different area upon weight bearing.
- Our doctors will offload the injected area by placing a felt pad either directly on the foot or in your shoe to help contain the fat injection to the area until your body converts it to fat through the processes of angiogenesis and adipogenesis, which takes 7-14 days.
- The patient can walk on the area afterwards once the offloading pad is applied.
- The maximum benefit from the injection will be reached by 10-12 weeks post- injection as by this time your body has converted all of the injected substance into fat.
How long does it last:
- There are a number of factors that determine the length of time that the fat will last including each patients weight, activity level and level of deformity but in general the injection will last 6 months to a year before it can be determined if any additional injections are needed.
Cost:
- Leneva injections are currently a cash service and not covered by insurance. The price varies based on the amount of fat that needs to injected which is determined by the area that is affected.
- We recommend that you call our office and schedule a Leneva consult to determine if you are a good candidate for a Leneva injection and what size injection would be indicated which will determine the cost.
It is estimated that 10% of the U.S. population will have heel pain at some point in their lifetime. Although there are many differential diagnoses for heel pain the most common is plantar fasciitis. The plantar fascia is a band of tissue on the bottom of the foot that connects the heel to the forefoot and helps to support the underlying plantar musculature or arch of the foot. Plantar fasciitis is an inflammatory condition in which there is pain and inflammation surrounding the insertion of the plantar fascia on the heel bone.

If you are in that lucky 10% of the population that has heel pain and you think it may be plantar fasciitis you may be wondering what to expect when you see your podiatrist. During you first visit your doctor will review you medical history and ask you specific questions about your heel pain that can help to confirm the diagnosis. One of these questions will be WHEN do you get the pain. If it is plantar fasciitis the pain should be the worst with the first couple steps in the morning or after getting up from sitting for a period of time. Your doctor will also likely take an x-ray of your foot to see if there are any fractures of heels spurs present. The presence or absence of a heel spur does not confirm or eliminate the diagnosis of plantar fasciitis but if there is a heel spur present it suggests that the plantar fascia is pulling on the heel bone at its insertion causing new bone to form… hence a heel spur.
Once your doctor has determined that you do indeed have plantar fasciitis he or she will review your treatment options. In my practice there are three tiers of treatment options:
Treatment Tier One:
- Change shoe gear to supportive shoes… no flats or heels!
- Avoid barefoot walking
- Stretch, stretch, stretch… I give patients a hand out of stretching exercises that help to improve plantar fascial symptoms. I emphasize stretching prior to getting out of bed in the morning in order to prevent those first painful steps.
- Anti-inflammatories – Since plantar fasciitis is an inflammatory condition this help to counteract the inflammation and alleviate pain.
- Icing – Again this aims at decreasing inflammation. A trick I tell patients is to freeze a water bottle and roll it under the arch for 20 minutes, 3 times daily.
Treatment Tier Two:
- Orthotics – these are arch supports that go inside the shoe to help prevent the arch from collapsing and the plantar fascia from tugging on the heel bone. These can either be over the counter or custom fabricated for your foot.
- Steroid injection – the purpose of the injection is to decrease the inflammation surrounding the plantar fascia and thus decrease pain.
- Physical Therapy – there are many physical therapy modalities that can help relieve plantar fasciitis including ultrasound therapy, graston therapy, and stretching and strengthening exercises. I normally have my patients go to therapy 2-3 times per week for 4-6 weeks.
Treatment Tier Three:
- Casting – In patients who are simply not improving with conservative treatments and want to avoid surgery I recommend casting the patient for 4 weeks to allow the plantar fascia to heal.
- Extracorporeal shock wave therapy – this options is not covered by insurance but can be useful in recalcitrant cases for plantar fasciitis.
- Surgery – A plantar fascial release is an effective treatment options when conservative options have been exhausted.
Plantar fasciitis can be a debilitating condition but in most cases it is only temporary and can be cured with conservative treatment options. Hopefully this blog has provided you with some basic concepts on plantar fasciitis and what to expect when you see your podiatrist.
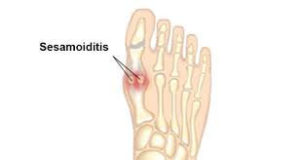
Sesamoiditis is a condition in which there is pain and inflammation surrounding the small bones under the big toe joint called the sesamoids. Most people have two sesamiods underneath the first metatarsal head called the tibial and fibular sesamoids. They are marble sized and shaped bones that sit on either side of the flexor tendons to the big toe. Because of their location these bones tend to take up a lot of force with activity since they are right at a weight bearing surface. If they become inflamed it is important to seek treatment as this is a condition in which early treatment can decrease the length of the condition.
Treatment for sesamoiditis consists of examination of the area and radiographs to rule out fracture or avascular necrosis (death of the bone), offloading with a surgical shoe or boot and R.I.C.E therapy. Sometimes special imaging may need to be ordered if the diagnosis is not straight forward.
Symptoms:
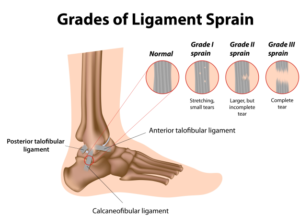
The primary symptoms of ankle sprains are swelling, bruising, and pain after a twist or injury to the area.
Treatment:
To heal properly, most ankle sprains require resting, elevating, and applying ice to the affected area to reduce swelling. Wrapping the ankle with compressive bandages to immobilize and support the ankle during healing may also help. More serious ankle sprains, often found in competitive athletes, may need surgery to repair or tighten damaged ligaments.
Prevention:
Exercising, stretching, and wearing shoes that fit well will help maintain foot and ankle strength, as well as maintaining balance and flexibility to help prevent ankle sprains.
Fracture Care:
There are several different types of possible breaks, or fractures, that you can experience in your foot and ankle. Rest assured that our office will treat your injury specifically. We’ll take an x-ray to determine whether the bone is fractured, or bruised.
If the bone is bruised, we’ll put you in a surgical shoe or walking boot. Rest, icing, compression, and elevation of the injured foot or ankle, along with anti-inflammatories will be prescribed until the pain subsides enough for you to return to normal activity.
If the bone is fractured, or broken, we’ll determine the severity of the break, and treat you accordingly.
For a stress fracture, you’ll likely be put in a walking boot or surgical shoe for approximately 4-6 weeks. For oblique or transverse fractures, where the broken ends are close to each other and will heal on their own, you’ll get a walking boot and crutches. More severe fractures require surgical intervention to realign the bone and help heal the break by putting in a pin, plate, or screws.
Make sure to follow all of your podiatrist’s instructions in order to ensure full healing.


Diabetic Foot Care:
Diabetes decreases blood flow, so injuries heal slowly. A foot wound as small as a blister from wearing tight shoes can lead to severe complications. According to the American Diabetes Association, almost 6 percent of the U.S. population has diabetes (5.9 percent, about 15.7 million people). Neuropathy, or nervous system damage, is a major complication that affects about 60 to 70 percent of diabetics, and may cause numbness, or the loss of feeling, in their feet or hands.
Diabetics are at a large risk for foot problems, and must constantly monitor their feet to avoid serious complications that can lead to amputation. Diabetics heal more slowly because of decreased blood flow, so small injuries can quickly become severe, as unhealed wounds are at increased risk for infection. Infections spread quickly in those suffering from diabetes, and can quickly become serious.
Diabetics need to inspect their feet every day for puncture wounds, bruises, pressure areas, redness, warm spots, blisters, ulcers, open sores, scratches, cuts, and problems with the nails. If you have a hard time seeing your feet, use a mirror, or have someone help you.
Neuropathy, or numbness, increases the risk of feet becoming deformed. Open sores can easily become infected, developing into ulcers. Neuropathy can also lead to Charcot foot (pronounced “sharko”), one of the most serious foot problems that can develop. Charco foot is caused by bones fracturing and disintegrating, warping the foot. The condition gets worse as you continue to walk on it because you can’t feel the pain.
Treatment:
Both foot ulcers and the early stages of Charco fractures can be treated using a total contact cast. The cast is molded from the shape of your foot, and is changed regularly, every one to two weeks, until your foot heals. In order to be effective, the contact cast requires good blood flow in the foot. The cast allows ulcers to heal by more evenly distributing weight, and relieving the pressure against the sore. In the case of Charco foot, the cast supports the foot, and controls movement. Charcot foot can also be treated with a custom walking boot, which supports the foot until the swelling goes down, a process that can take up to a year. With both the contact cast and walking boot, you should try to keep from putting weight on the affected foot. If the warping of the foot is too severe for a brace, cast, or shoe, surgery may be considered.

Venous Insufficiency is a disorder of the veins, typically of the lower extremities, in which they are not pumping the blood back up to the heart as efficiently as they are supposed to. Unlike arteries, veins have one-way valves which help to pump the blood against gravity up to the heart. In a patient with venous insufficiency these valves are not working properly any more so blood pools in the lower extremities. As blood pools in the legs it causes swelling, bulging veins and skin changes. If this disease process continues for long enough people with venous insufficiency can develop ulcerations of the skin. Venous ulcerations can be very painful and need to be treated by a medical professional immediately. Compression therapy is the standard of care of venous ulcerations as the real issue is the swelling in the legs. Without treating the swelling, the ulcerations will not go away. If left untreated venous ulcerations can become quite large and become infected. Make an appointment today if you think you are suffering from venous Insufficiency or venous ulcerations.
Ganglion cysts are one of the most common masses to develop on the foot and ankle. They are fluid filled sacs that protrude from a joint or tendon sheath. These lesions tend not to be painful unless they become large enough that they affect surrounding nerves or interfere with shoe gear. If you think you have a ganglion cyst it is important to have it evaluated as a definitive diagnosis is imperative to make sure the mass is not something malignant. When you come to your visit the podiatrist will exam the mass to determine its texture, mobility and location. Ganglion cysts tend to be soft, mobile and near a joint or tendon. In most cases ganglion cysts can be aspirated or drained to deflate the lesion and get a sample of the fluid inside to send to pathology to confirm the diagnosis of ganglion cyst. In some cases when a cyst is drained is does not return but in other instances it can fill back up and return. When you have a recurrent cyst sometimes it needs to excised to remove not only the fluid but also the sac.

Metatarsalgia is a condition in which patients feet pain and fatigue to the bottom ball of the foot. This tends to be an overuse condition that is triggered by a change in activity or a change in shoe gear. There are some factors that increase your risk of metatarsalgia including improper shoe gear (i.e. high heels), decreased fat pad to the ball of the foot and a high arched foot. All of these stated factors increase the pressure on the metatarsal heads which can lead to pain and fatigue. It is important to have metatarsalgia evaluated as in some cases if the pressure is not alleviated to the metatarsals then large painful calluses can form a stress fracture can develop.


A neuroma is a thickening or enlargement of nerve tissue that can lead to tingling, burning, numbness, pain and other discomfort. Neuromas, thickening of the nerve tissues, can develop all over the body. The most common neuroma in the foot is called a Morton’s neuroma, sometimes called an intermetatarsal neuroma, and develops between the third and fourth toes. However, neuroma’s can develop in other places on the foot as well. Compression and irritation to the nerve cause the thickening, or enlargement of the nerve, and can lead to permanent nerve damage if left untreated.
Symptoms:
Neuromas can cause tingling, burning, numbness, pain, or the sensation that something is inside the ball of the foot, or that something is bunched in the shoe or sock. Symptoms usually begin gradually, only appearing occasionally, usually when wearing narrow-toed shoes, or doing certain activities. The symptoms may go away when the shoe is removed, or the foot is massaged. Over time, however, the symptoms worsen and the discomfort can last for several days or weeks at a time. The symptoms become more intense as the neuroma enlarges and the changes in the nerve become more permanent. See your podiatrist as soon as you notice symptoms–the earlier the diagnosis, the less the need for invasive treatments or surgery.
Causes:
Anything causing compression or irritation of the nerve can lead to a neuroma developing. Wearing tight shoes, shoes with narrow toe boxes, or high-heeled shoes that squish the toes are the main causes of neuroma development. Some foot deformities, like bunions, hammertoes, flatfeet, or flexible feet, provide a higher risk for developing a neuroma. Activities involving repetitive irritation to the ball of the foot, like running or court sports, can also lead to neuromas. Sometimes, neuromas can develop after an injury or other trauma to the area.
Treatment:
Treatment options depend on how long you’ve had the neuroma, and on its developmental stage, and vary depending on the severity of the neuroma.

Arthritis is a inflammatory disease of the joints. The foot has 33 joints and thus there is a lot of room for arthritis to develop! Some of the most common areas that we see arthritis in the foot are the big toe joint, ankle joint and midfoot joints. An x-ray will be taken at your appointment to access the amount of arthritis in the joints. Conservative treatment of arthritis to the foot and ankle can consist of bracing, orthotics, NSAIDs, steroid injections or topical medications. Sometimes conservative therapy is not enough and surgical intervention is need to alleviate the pain from arthritis in the foot.


Toenail fungus AKA onychomycosis is a fungal infection of the toenails. This is one of the most common pathologies affecting the feet with an estimated 10-20% of the US population being affected. Just like any condition there are different degrees of severity to this conditions and thus different treatment options. It is important to see a podiatrist right away if you think you have contracted a toenail fungus infection as the sooner treatment begins the more successful it can be. The first thing that will be done in the podiatrist’s office is to confirm that you actually have a fungal infection. This is done by taking a sample of the infected nail and sending it off to a lab that will look at it under the microscope to determine if there is fungus and what type of fungus is present. With this knowledge treatment can then be tailored to your needs. Treatment for toenail fungus consists of debriding the affected nails to get as much excess fungal debris out as possible followed by either topical anti-fungal therapy, oral anti-fungal therapy, nail removal or laser nail therapy. Sometimes combinations of the fore-mentioned therapies are utilized. Make an appointment with us today to find out what the most appropriate treatment options is for your toenail fungus.
Warts of the foot, AKA plantar warts or verruca plantaris, are a viral infection caused by the Human Papillomavirus (HPV). Plantar warts can affected people of all ages but tend to be more common in adolescence or immunocompromised individuals. These lesions present as either a solitary wart or a cluster or warts called a mosaic wart. They tend to be painful with side to side compression, have an absence of skin lines through the lesion, and have small black dots in the center called “hyphae” which are actually dry blood contained within the capillaries of the wart. If you think you have a wart you should consult with your podiatrist right away as warts not only can multiply but can also spread from person to person by contact. When you come to the podiatry office your doctor will talk to you about the different treatment options for plantar warts including topical kerolytics (AKA cantharidin or salycyclic acid, the ingredient found in most over the counter medications), cryotherapy, or laser therapy.

The above picture depicts a plantar wart. Notice the absence of skin lines through the wart as well as the central hyphae. These clinical clues help determine that this lesion is a wart.

Ingrown toenails, also known as Onychocryptosis, are one of the most common pathologies that podiatrist treat. The first thing to realize about ingrown toenails is that they are not all created equal and so they are not all treated the same. There are different stages to ingrown toenails ranging from an irritated ingrown toenail to an infected ingrown toenail. The most important thing to remember is DON’T WAIT to come into the office if you think you have an ingrown toenail. There are treatment options when an ingrown toenail first presents that cannot be used if the ingrown toenail is more advanced.
An ingrown toenail happens when the nail curves and grows into the skin, usually at the sides of the nail. When the nail digs into the skin, it causes irritation and often leads to pain, redness, swelling, and warmth in the toe. If an ingrown nail causes a laceration, or cut, in the skin, it can become infected. Some signs of infection are drainage or pus, and a foul odor. Even if you don’t notice any pain, swelling, redness, or unusual warmth, an ingrown toenail can still become infected, and needs to be taken care of.
Depending on the severity of the ingrown toenail the nail may either be cut back with or without local anesthetic. Sometimes patients will need to be put on an oral antibiotic if the surrounding soft tissue is infected. After the nail border is removed the patient will be instructed to soak in Epsom salts and water daily and apply antibiotic ointment and a bandaid.
Causes:
The most common cause of ingrown toenails is cutting your toenails too short, or cutting them incorrectly. Improper trimming can damage the nail. The skin will fold over the nail, making the nail grow into the skin, or become “ingrown.” Other causes come from pressure or trauma, and in some cases, there may be a hereditary predisposition for ingrown toenails. Excessive pressure on the toenail, from shoes, or repeated kicking or running, can also cause the nails to dig into the skin. Trauma, such as stubbing your toe, or having a heavy object fall on your toe, can sometimes cause an ingrown toenail.
Wearing socks or shoes that are too tight, or too short, can cause ingrown toenails because of the pressure on the toes. Ingrown toenails can also be caused by fungal infections, or by losing a nail. Bone deformities of the toes can change the shape of toenails, and also lead to them becoming ingrown.
Treatment:
Home care:
Home treatment for ingrown toenails is strongly discouraged if an infection is suspected, or for those who have medical conditions such as diabetes, nerve damage in the foot, or poor circulation that put feet at high risk. If you don’t have an infection or any medical conditions affecting your feet, you can soak your foot in room-temperature water (adding Epsom’s salt if recommended by your doctor), and gently massage the side of the nail to help reduce the swelling. DO NOT attempt “bathroom surgery,” or to cut the toe out of the skin at all. Repeated cutting of the ingrown toenail can make condition worse over time. If your symptoms don’t improve with soaking or over time, see your podiatrist.
Physician care:
Oral antibiotics may be prescribed to help treat infection; however, antibiotics alone cannot cure an infected ingrown toenail. The infection will continue to return until the nail is fixed, and no longer digs into the skin. A minor surgical procedure can often be done in the office, to remove the nail and ease the pain. After applying a local anesthetic, the podiatrist removes the ingrown part of the nail. For nails that repeatedly become ingrown, there’s a more permanent option. The podiatrist can remove the nail matrix, the area responsible for nail production, and prevent further ingrown toenails. This procedure is still minor, and is often done in the office. The toe is wrapped in a light bandage after the procedure, and most people resume normal activity the next day, experiencing very little pain after surgery. If you’ve been prescribed an oral antibiotic, be sure to take all the medication even if your symptoms have improved.
Prevention:
Ingrown toenails can be prevented by properly trimming toenails, and by wearing appropriate footwear.
When trimming, cut toenails in a straight line, avoid rounding the nail, and don’t cut them too short. They should be long enough so that you can get your fingernail under the sides and end of the nail.
Wear shoes and socks that fit properly. Don’t wear shoes that are short or tight in the toe area. Also avoid shoes that are loose, because they can cause pressure on the toes, especially during running or brisk walking.


Athlete’s foot is a chronic fungal infection, and is most often contracted in places like locker rooms, public showers, swimming pools, or anywhere else where people go barefoot.
Several different types of fungus can cause Athlete’s foot, which can range from mild scaling and itching, to painful swelling, inflammation, and blisters. It often begins between the toes, or on the arch of the foot, but can spread to the bottom and sides.
Treatments:
Successful treatment requires a combination of medication and self-care. The kind of medication required depends on the type of infection, since there are different kinds of fungus that cause Athlete’s foot. Over-the-counter or prescription powders, lotions, and ointments are available to treat scaling, itching, and inflammation for less serious cases. Soaking the foot may help resolve excessive perspiration. Make sure to consult your physician before taking any medication or beginning treatment. If the Athlete’s foot does not improve with treatment, stronger medications may be required. Consult your podiatrist!
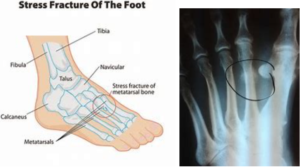
Stress fractures are a relatively common issue that occurs with the foot. It is possible to get a stress fracture in any bone of the foot but one of the most common bones we see stress fractures in is the metatarsals. Stress fracture are when the inner core of the bone (medullary bone) is fractured but the out cortical bone is still intact. Stress fractures normally develop after an increase in activity or change in shoe gear and can cause pain and swelling to the affected area. It is very important to seek treatment if you think you have a stress fracture in order to be properly immobilized and prevent a complete fracture from occurring.
Flatfeet
Flatfoot in children or pediatric pes planus is one of the most common etiologies that parents will bring their children to see the podiatrist about. Pediatric flatfeet can be broadly divided into two classes: symptomatic vs asymptomatic flatfoot. When you visit your podiatrist they will ask a number of questions that will help determine which class of flatfoot your child has. If the child has no pain, is neurodevelopmentally normal, hitting normal milestones with development, no history of excessive tripping then they are considered to have a asymptomatic flatfoot and in most cases will just be monitored. If the child has pain to the feet, any history of neurological or developmental impairment, is not hitting their normal developmental milestones on time or have an excessive history of tripping then they may need further workup to rule out any other underlying etiologies. We commonly give these symptomatic pediatric flatfoot patients custom orthotics or AFO braces to help allow them to function normally and eliminate their pain.

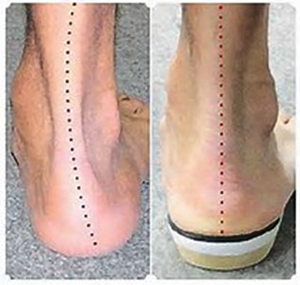

The pictures above show how an orthotic device can hold the foot in the correct functional position and prevent excessive pronation of the foot or rolling in of the arch.
In-toeing

Sometimes called “pigeon-toed”, in toeing is a condition in which the toes point inwards towards on another. It is important to see a podiatrist to evaluate why you are having intoeing as there are different causes. The major causes of intoeing are metatarsus adductus, interneal tibial torsion and femoral anteversion….. basically the intoeing is either coming from the foot bones, lower leg bone or thigh bone. In most cases intoeing is noticed in pediatric patients. Kids tend to grow out of this positioning deformity with age and growth but in some cases intervention, physical therapy of casting is needed.
Toe Walking

Toe-walking is a condition that tends to occur in early childhood. Sometimes the child will start out toe-walking from the beginning but other times children will learn to toe walk over time. It is important with this condition to be evaluated as sometimes toe walking can be a sign of an underlying neuromuscular disorder. In many cases toe walking is simply a learned behavior in which the child needs to be conditioned not to perform the behavior any more. The risk of not treating toe walkers is that they will develop contractures to the achilles tendon and require surgery or serial casting to re-lengthen this tendon.
Curly Toes
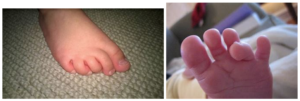
Curly toes are a deformity of the toes in which the toes curl towards the big toe. This most commonly affected the 4th toe but can also affect the 2nd or 5th toes. This tends to occur in early childhood from a tend imbalance in which the flexor tendon is overpowering the extensor tendon. In some cases people will out grow there curly toe deformity as they grow but in other cases surgical intervention may be necessary to prevent blistering, sore, pain with shoe gear or future arthritic changes to the toe joints.
Ingrown Toenails

Ingrown toenails, also known as Onychocryptosis, are one of the most common pathologies that podiatrist treat. The first thing to realize about ingrown toenails is that they are not all created equal and so they are not all treated the same. There are different stages to ingrown toenails ranging from an irritated ingrown toenail to an infected ingrown toenail. The most important thing to remember is DON’T WAIT to come into the office if you think you have an ingrown toenail. There are treatment options when an ingrown toenail first presents that cannot be used if the ingrown toenail is more advanced.
An ingrown toenail happens when the nail curves and grows into the skin, usually at the sides of the nail. When the nail digs into the skin, it causes irritation and often leads to pain, redness, swelling, and warmth in the toe. If an ingrown nail causes a laceration, or cut, in the skin, it can become infected. Some signs of infection are drainage or pus, and a foul odor. Even if you don’t notice any pain, swelling, redness, or unusual warmth, an ingrown toenail can still become infected, and needs to be taken care of.
Depending on the severity of the ingrown toenail the nail may either be cut back with or without local anesthetic. Sometimes patients will need to be put on an oral antibiotic if the surrounding soft tissue is infected. After the nail border is removed the patient will be instructed to soak in Epsom salts and water daily and apply antibiotic ointment and a bandaid.
Causes:
The most common cause of ingrown toenails is cutting your toenails too short, or cutting them incorrectly. Improper trimming can damage the nail. The skin will fold over the nail, making the nail grow into the skin, or become “ingrown.” Other causes come from pressure or trauma, and in some cases, there may be a hereditary predisposition for ingrown toenails. Excessive pressure on the toenail, from shoes, or repeated kicking or running, can also cause the nails to dig into the skin. Trauma, such as stubbing your toe, or having a heavy object fall on your toe, can sometimes cause an ingrown toenail.
Wearing socks or shoes that are too tight, or too short, can cause ingrown toenails because of the pressure on the toes. Ingrown toenails can also be caused by fungal infections, or by losing a nail. Bone deformities of the toes can change the shape of toenails, and also lead to them becoming ingrown.
Treatment:
Home care:
Home treatment for ingrown toenails is strongly discouraged if an infection is suspected, or for those who have medical conditions such as diabetes, nerve damage in the foot, or poor circulation that put feet at high risk. If you don’t have an infection or any medical conditions affecting your feet, you can soak your foot in room-temperature water (adding Epsom’s salt if recommended by your doctor), and gently massage the side of the nail to help reduce the swelling. DO NOT attempt “bathroom surgery,” or to cut the toe out of the skin at all. Repeated cutting of the ingrown toenail can make condition worse over time. If your symptoms don’t improve with soaking or over time, see your podiatrist.
Physician care:
Oral antibiotics may be prescribed to help treat infection; however, antibiotics alone cannot cure an infected ingrown toenail. The infection will continue to return until the nail is fixed, and no longer digs into the skin. A minor surgical procedure can often be done in the office, to remove the nail and ease the pain. After applying a local anesthetic, the podiatrist removes the ingrown part of the nail. For nails that repeatedly become ingrown, there’s a more permanent option. The podiatrist can remove the nail matrix, the area responsible for nail production, and prevent further ingrown toenails. This procedure is still minor, and is often done in the office. The toe is wrapped in a light bandage after the procedure, and most people resume normal activity the next day, experiencing very little pain after surgery. If you’ve been prescribed an oral antibiotic, be sure to take all the medication even if your symptoms have improved.
Prevention:
Ingrown toenails can be prevented by properly trimming toenails, and by wearing appropriate footwear.
When trimming, cut toenails in a straight line, avoid rounding the nail, and don’t cut them too short. They should be long enough so that you can get your fingernail under the sides and end of the nail.
Wear shoes and socks that fit properly. Don’t wear shoes that are short or tight in the toe area. Also avoid shoes that are loose, because they can cause pressure on the toes, especially during running or brisk walking.
Warts
Warts of the foot, AKA plantar warts or verruca plantaris, are a viral infection caused by the Human Papillomavirus (HPV). Plantar warts can affected people of all ages but tend to be more common in adolescence or immunocompromised individuals. These lesions present as either a solitary wart or a cluster or warts called a mosaic wart. They tend to be painful with side to side compression, have an absence of skin lines through the lesion, and have small black dots in the center called “hyphae” which are actually dry blood contained within the capillaries of the wart. If you think you have a wart you should consult with your podiatrist right away as warts not only can multiply but can also spread from person to person by contact. When you come to the podiatry office your doctor will talk to you about the different treatment options for plantar warts including topical kerolytics (AKA cantharidin or salycyclic acid, the ingredient found in most over the counter medications), cryotherapy, or laser therapy.

The above picture depicts a plantar wart. Notice the absence of skin lines through the wart as well as the central hyphae. These clinical clues help determine that this lesion is a wart.
Calcaneal Apophysitis (Severe’s Disease)
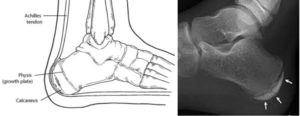
Calcaneal Apophysitis (also known as Sever’s Disease) is a painful inflammatory condition that most commonly affects children aged 8-14. The inflammation in this condition is centered around the calcaneal growth plate (heel) and tends to cause symptoms such as heel pain and limping. The cause of this condition is increased tension on the growth plate from repetitive trauma and tugging of the achilles tendon on the insertion of the growth plate. There are many treatment options for calcaneal apophysitis including offloading the heels with gel heel pads, crutches or a walking boot as well as rest, NSAIDs and physical therapy.

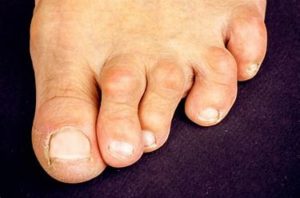
Bunions are a deformity in the foot where the joints in the big toe are misaligned. The first big toe joint bulges out, away from the foot, and the second joint angles in towards the other toes. The joints can become sore and swollen, and make shoes fit improperly and uncomfortably.
The deformity causing a bunion is in the bone, an enlargement of the joint at the outside bottom of the big toe (the metatarsophalangeal joint). Bunions form when the toe moves out of place. The bump caused by the enlargement of the joint can rub uncomfortably against footwear, creating friction and pressure. Left untreated, the big toe’s movement angles in towards the other toes, and can sometimes overlap other toes (called Hallux Valgus). The movement causes the protuberance, or bump, to grow, which leads to increased irritation and inflammation. Sometimes, the big toe rotates, or twists, as it moves towards the second toe (known as Hallus Abducto Valgus). Bunions can also develop into other toe deformities like hammertoe.
The toe joint is always moving and flexing with every step, and the constant irritation, rubbing, and friction of bunions against footwear cause many people with bunions to suffer discomfort and pain, especially while walking, which increase as the bunion grows. The skin on the affected toe can become red and tender. Eventually, the deformity in the joint can lead to bursitis or arthritis. The skin on the bottom of the foot can thicken, and walking can become increasingly difficult. Untreated, bunions can lead to chronic pain.
Causes:
Bunions are mainly caused by wearing shoes that are too tight. Although bunions are not strictly hereditary, they do seem to run in families, usually because of faulty foot structure. Foot injuries, neuromuscular problems, flat feet, and pronated feet can all lead to bunion formation. 33% of people in Western countries are estimated to suffer from bunions.
Treatment:
Because bunions are bone deformities, they will not resolve on their own. The goals for bunion treatment are to relieve the pressure and pain caused by irritation, and to halt the growth of the enlargement. The most common methods to reduce pressure and alleviate pain include:
- Protective padding: Usually made from felt material, the padding can alleviate the inflammation and skin problems from the pressure and friction of the bunion against shoes.
- Remove corns and calluses: Removing corns and calluses on the foot can also reduce friction and pressure, helping shoes fit more appropriately, and alleviating some of the pain.
- Special footwear: Footwear designed specifically to accommodate the bunion without contributing to its growth can prevent it from getting worse, and can alleviate pain and pressure.
- Orthotic devices: Available both over-the-counter or custom made, orthoses can help to stabilize the affected toe joint, and keep the foot in a comfortable position for walking and standing.
- Exercise: Regular exercise of the affected area will help to maintain joint mobility and prevent stiffness or arthritis.
- Splints: Worn at night , splints can help realign the affected toes and joint. Adolescents suffering from bunions often benefit from this treatment, since their still-developing bones are more adaptable.
Flat feet are a common condition. The arch in the bottom of the foot continues to develop during childhood. Flat feet are normal in infants and toddlers, since the longitudinal arch is not yet developed. By adulthood, most people have developed normal arches.
Generally, flat feet are associated with pronation, where the ankle bones lean in towards the center of the body. Shoes belonging to children who pronate (after they’ve been worn long enough to be remodeled by the child’s foot) will lean toward each other when they are placed side by side, demonstrating the pronation.
Symptoms:
Many people with flat feet do not experience any pain or other problems from their flat feet. If pain in the foot, ankle, or lower leg does occur, especially in children, the feet should be evaluated.
Complications:
Flat feet or an abnormal tendon attachment in the foot can lead to a predisposition for tibialis posterior tendonitis, otherwise known as painful progressive flatfoot, or adult-acquired flatfoot, where the tendon at the back of the ankle (the tibialis[N1] posterior) becomes inflamed, stretched, or torn. If left untreated, tibialis posterior tendonitis may lead to severe disability and chronic pain.
Treatment:
Common treatments for tibialis posterior tendonitis are nonsteroidal anti-inflammatory medications, icing, physical therapy, supportive taping, bracing, and orthotic devices. Note: Please consult your physician before taking any medications. In some cases, surgery may be required to repair a torn or damaged tendon. In the most severe cases, operating on the bones of the foot to treat the flatfoot condition may be necessary.
A deformity in the second, third, or forth toe that causes the toe to bend at the middle joint, making it look like a hammer, is called hammertoe. Hammertoes can lose flexibility, and deteriorate to the point of needing surgery if they are left untreated.
Symptoms:
Hammertoe is a deformity or bending of the middle toe joint that makes it look like a hammer. Some complications of hammertoe include corns or calluses above the middle joint of the affected toe, or on the tip of the toe. Other complications include pain in the toes or feet, and difficulty in finding comfortable shoes.
Causes:
Hammertoe may be caused by muscle imbalance, and by wearing shoes that don’t fit well.
Treatment:
If caught early enough, hammertoe can be treated by wearing shoes that are soft and roomy in the toe area, and by performing exercises to stretch and strengthen the affected muscles. Straps, cushions, or non-medicated corn pads, available over-the-counter, can also help alleviate discomfort.
Severe cases may require surgery.
- Keep your feet warm.
- Avoid getting your feet wet in snow or rain.
- Don’t put your feet on radiators or in front of the fireplace.
- Don’t smoke, and don’t sit cross-legged. Both decrease blood supply to your feet.
- Don’t soak your feet.
- Don’t use antiseptic solutions, drugstore medications, heating pads, or sharp instruments on your feet.
- Cut your toenails straight across; avoid cutting the corners. Use a nail file or emery board instead of clippers or scissors. If you find an ingrown toenail, contact your podiatrist
- Moisturize the skin on your feet with good quality lotion, but avoid getting any lotion between your toes.
- Wash your feet with mild soap and warm water daily.
- Wear loose socks to bed.
- Wear warm socks and shoes on cold days.
- Pat each foot dry with a towel, making sure to carefully dry between the toes.
- Buy shoes that are comfortable even before they are “broken in.” Make sure they fit widthwise and lengthwise, at the back, bottom of the heel, and at the sole. Avoid shoes with pointed-toes or high heels. Shoes with leather uppers and deep toe boxes are better. While breaking in shoes, wear the new shoes for a maximum of two hours at a time.
- Alternate your shoes: don’t wear the same pair every day. Check the inside of each shoe for rips, tears, or anything that could cause friction and rub against your feet, causing blisters or irritation. Don’t lace your shoes too tight or too loose.
- Wear appropriate socks and stockings. Wear clean, dry socks every day. Do not wear wrinkled socks, or socks with holes in them. Thin cotton socks are more absorbent, and will keep your feet dry, especially on warm days. Socks with square toes are roomier, and will not squeeze your toes. Do not wear socks or stockings with elastic tops.
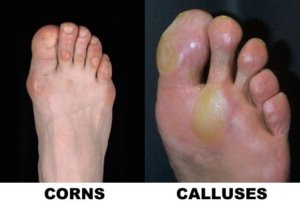
Corns and calluses are thick layers of compressed dead skin cells that develop to protect the skin. They are caused by repeated friction against bony areas of the foot, or from shoes rubbing against the skin. Calluses form on the bottoms, or soles of the foot, and corns on the toes.
Treatment:
The pain or burning from the friction and pressure against the skin can be alleviated by padding the affected areas, or by using moleskin. Never cut corns or calluses, and never use home remedies without a podiatrist’s instructions.

A podiatrist can prescribe orthotic inserts to help alleviate the problems associated with many different food conditions.Conditions like Pediatric flatfoot, neuromas, heel pain, PTTD, and flexible flatfoot can be helped with orthoses. These custom shoe inserts are created using a plaster mold of the foot, and support and align the foot and lower extremities so that the foot, leg, and hips are all aligned as they should be. Be careful of buying premade orthotic devices over-the-counter. Using orthotic inserts not made for your foot, or your specific situation, can make foot problems worse. Talk to your podiatrist before using any shoe inserts.

Laser Nail Treatment is a new way to treat an old problem, and can be used to treat some cases of athlete’s foot or other fungal infections. It works by using laser light to prevent the fungus from growing and spreading, and stopping the nail from becoming thick and yellowed. After the fungus is killed, the nail will take some time to grow out, usually six to nine months, but will grow back clean and fungus free. Laser nail treatment takes the same amount of time as other antifungals, but provides a safer, more efficient treatment because no medication is required. There are no side effects with laser nail treatment that can be present with medication.
Foot pain can be caused by various complications, such as neuromas, hammertoe, bunion, capsulitis, fractures, etc., and is never fun to live with. Our office will make sure to treat your specific condition in the best possible manner. Upon your visit, your podiatrist will pinpoint the location where you’re experiencing the pain, and assess the type of pain you’re feeling. Diagnostic tests such as x-rays, injections, and biomechanical measurements may be used to determine the specific complication, and to best decide the course of treatment. Your treatment will depend on your specific condition, and can range from recommending rest and medication, prescribing orthotics, to surgical intervention. Don’t live with your foot pain. Simple conditions can often become worse and lead to further complications. Our office can help you manage your foot pain, and get you comfortably back on your feet, both physically, and emotionally.

Brachymetatarsia is a congenital condition in which one or more of the metatarsal bones of the foot are shorter then it is suppose to be. This most commonly affects the 4th metatarsal but can also affect the other metatarsals as well. Although the metatarsal is short, this deformity actually gives the appearance of a short toe. The only way to fix this deformity is with a reconstructive surgery that lengthens the metatarsal bone over time. Since this is an extensive procedure it is only recommended to undergo this procedure if there is pain associated with the short toe and not just for cosmetic reasons.
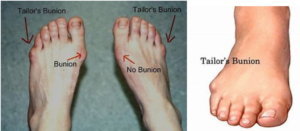
Tailors bunion (AKA bunionette) is a come foot deformity in which there is a bump on the side of the foot just before the 5th toe which leaves people with a wide foot. This deformity can cause pain from rubbing in she gear or callusing under the 5th metatarsal head. There are conservative and surgical treatment options for this deformity. Conservative options consist of padding up and accommodating the deformity with different toe pads and wider shoe gear. Surgical treatment consists of both soft tissue and bony surgery to correct the deformity. Speak to one of our podiatrists to find out what the best treatment option is for your foot.
There are many questions surrounding diabetic wound care and treatment. Especially as it relates to diabetic wound care of the foot. Dr. Natalie Domek with Podiatry of Chicago specializes in diabetic wound care of the foot and has provided some information to help keep you informed and on your feet.
-
- According to the American Diabetes Association the incidence of diabetes in the United States is approaching 10%
-
- 34% of diabetics will develop a foot ulceration
-
- After healing a diabetic foot ulceration the reoccurrence rate is 40% in the first year alone
- Treatment options:
-
- Wound debridement (in office vs in surgery)
-
- Antibiotic therapy (if indicated)
-
- X-rays to rule out underlying bone infection
-
- Lab work to determine if there is any underlying reasons why the wound may not be healing (i.e. low albumin, high HbA1c, high CRP or ESR levels)
-
- Peripheral Arterial disease workup…. Do you have enough blood flow to heal your wound
-
- Offloading – total contact casting vs surgical shoe vs CAM boot vs offloading pads vs diabetic inserts
-
- Home health orders for dressing changes
-
- Edema (swelling control)
-
- Unna boot wraps
-
- Lymphedema pumps
- Jones compression dressings
-
- Edema (swelling control)
- Advanced wound care products
-
- Collagen products
- Skin substitute products

-
- Epifix
-
- Amniofix
- Grafix
-
-
-
For more on diabetic wound care and complications also see: Podiatry of Chicago Diabetic Wound Care Services
